Anosmia
By Dr Hannah Missen
Is it the End of the Nose after COVID-19?
We use our sense of smell every day in so many different ways.
It helps us taste food and drink, to detect things that might harm us (from sniffing milk to check if it’s off, to smelling smoke indicating a fire) and also plays a part in our memory, mood and emotion. A loss of sense of smell (anosmia) has been something many of us have been more familiar with since the COVID-19 pandemic.
Around 60% of those infected with COVID report a loss or change in sense of smell, but there are lots of other reasons why you might notice a change to this important sense.
Aside from anosmia, some people may experience parosmia (a change in sense of smell) or phantosmia (smelling things that aren’t there, like smoke or burnt toast). It’s also important to note that it’s really common to lose some sense of smell as you get older, too.
Let’s talk about some common reasons why your sense of smell might have changed. As we’ve already said, over half of people with COVID notice an effect on their sense of smell.
For most people it returns to normal after 2-3 weeks, but 1/10 will have longer lasting effects for 8 weeks or longer. The exact mechanism of why COVID affects smell isn’t entirely understood, but is thought to be related to damage to the cells that help the support and assist the nerves that live in our nose to detect smells and relay the information to our brain. The good news is that these cells can regenerate.
Other viruses, like colds and flu, can also have similar effects.
Obviously, by being bunged up with a snotty nose you might notice that your sense of smell is affected, but possibly mechanisms as with COVID might be at play. Symptoms, on the whole, tend to be less profound than with COVID and often return to normal within a week.
Rinsing the inside of your nose can help if you have an infection or allergy affecting your sense of smell. You can buy various kits and mixtures from the pharmacy to help you to do this, but you can also just do it yourself at home.

Sinusitis and allergies, like hay fever, can cause inflammation in your nose and can cause issues with your sense of smell too.
If you have allergies that cause nasal congestion, avoiding triggers is a big help. Using the above technique can alleviate symptoms, as can antihistamine tablets or sprays, or even steroid sprays if your symptoms don’t settle.
Sinusitis can be acute or chronic.
Acute sinusitis is rarely caused by bacteria; 98% of cases are caused by viruses. For this reason, antibiotics are not even considered until you have had symptoms for at least 10 days. Symptoms normally get better in 2-3 weeks, but if you haven’t started to improve after 10 days, nasal steroid sprays or sometimes antibiotics might be considered.
Chronic sinusitis can last for some months, and stopping smoking or avoiding allergic triggers can really help. The above technique or steroid nose sprays might also be helpful.
Nasal polyps are fleshy growths inside your nostril that can sometimes affect your sense of smell. They can also bleed, or cause a runny nose, but not always. Your GP can see if you have polyps by looking inside your nose with a light. Steroid drops and sprays often help, but if they don’t resolve it you might be referred to an Ear, Nose and Throat (ENT) specialist.
We know of all the damage that smoking, alcohol and illicit drug use (especially cocaine) can wreak on our organs. However, they are often overlooked as reasons for a change in smell, but are really important to consider. If you’re over 40 and live in Staffordshire, you can access stop smoking services by calling 03330 050095 or texting QUIT to 60777.
There are many, rarer, causes of changes to your sense of smell including head injuries, previous surgery, and medication. Cancers of the nose or brain are very uncommon reasons for changes to your sense of smell.
Many don’t realise the profound psychological impact that smell disorders can have. The impact on the sense of taste can affect appetite and subsequently cause weight loss and the physical health problems that go alongside this.
If you are affected by a loss or change in your sense of smell that doesn’t go back to normal after a few weeks, it is worth seeing or speaking to your GP. In particular, please ensure you seek medical attention as soon as you can if you have one-sided congestion in your nose, persistent headache, nose bleeds, crusting of your nostril, visual symptoms, smelling a ‘bad’ smell that isn’t really there, or weight loss.
Remember that you might not notice the smell of smoke in your home or sense that food is off, so ensure that your smoke alarms are working and that you label food carefully.
Depending on your symptoms and their duration, and clinical examination, you might be offered treatment by your GP, referred to ENT, or be given some things to try at home.
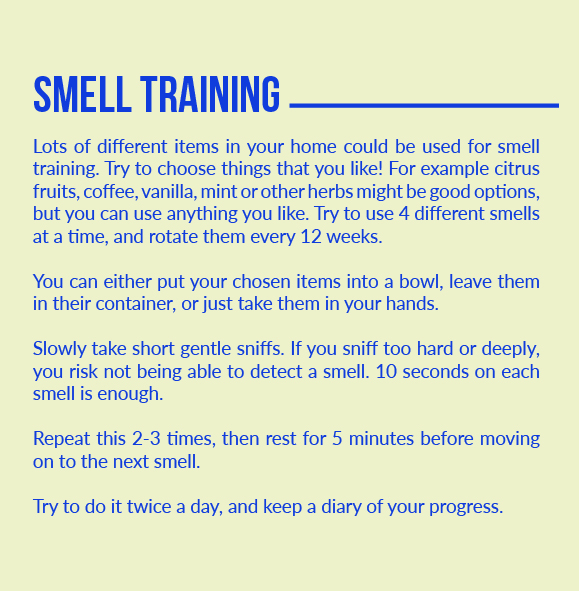
The Fifth Sense website has some really good resources regarding smell training, and not only can you buy commercially available kits to do this, but you can also use what you have at home. It includes a diary so that you can record your baseline sense of smell, and your progress. The Snif App from Abscent can also guide you through the process.
Even if progress is slow, it’s not the end of the nose. Please seek help if things aren’t getting back to normal, and be honest about the impact that your symptoms are having on your life, help is at hand.
Some good resources to look at for yourself include:
www.fifthsense.org.uk
www.yourcovidrecovery.nhs.uk
abscent.org
snif.abscent.org
Dr Hannah Missen is a mummy to Primrose, and a general practitioner (GP) with a previous background in obstetrics and gynaecology. She has particular interests in research and academia, medical ethics and law, and women’s health.
Find her on Twitter @DrMissen